When we talk about diseases, our minds usually jump to viruses, bacteria, or even parasites. But imagine a disease caused by something far more baffling: a protein. Yes, a protein – one of the building blocks of life – can turn rogue and wreak havoc, leading to devastating brain illnesses like the infamous “Mad Cow Disease.” These mysterious culprits are called prions, and they represent a silent, deadly threat that has puzzled scientists for decades.
What Exactly Are Prions? Not Alive, Yet So Deadly
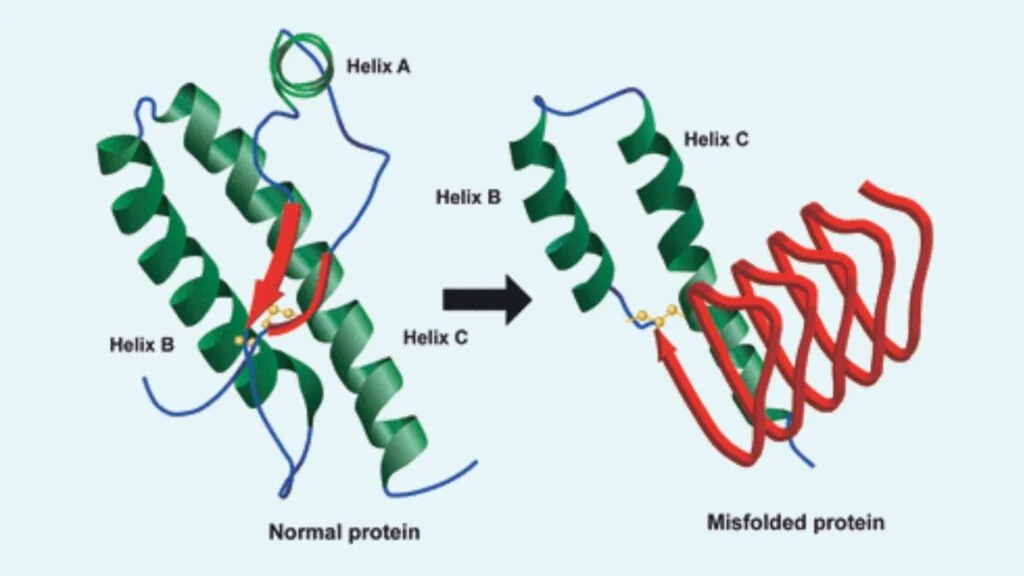
Forget what you know about typical infections. Prions are not living organisms. They don’t have DNA or RNA like viruses or bacteria. Instead, a prion is simply a normal protein in our bodies or in animals that has folded itself into the wrong shape. Think of it like a perfectly good piece of fabric that suddenly gets crumpled and won’t straighten out. The real danger begins when this misfolded, abnormal prion comes into contact with other healthy, normal proteins. It’s like a bad apple in a basket, but this bad apple actually forces all the good apples to turn bad too!
This misfolded prion acts like a template, forcing its healthy neighbours to also change into its abnormal, disease-causing shape. This process creates a chain reaction, leading to an unstoppable buildup of these corrupted proteins, especially in the brain. Over time, these abnormal proteins clump together, damaging brain cells and creating tiny holes, making the brain look like a sponge under a microscope. This is why these diseases are often called “spongiform encephalopathies.”
The Silent Threat, Years of Incubation, Then Disaster
One of the most frightening aspects of prion diseases is their long incubation period. An animal or a person can be infected with prions and show absolutely no signs of illness for years, sometimes even decades. During this silent phase, the rogue proteins are slowly, insidiously multiplying and destroying brain tissue. By the time symptoms finally appear, the damage is usually extensive, and the disease progresses rapidly.
What Are The Symptoms of Prions Disease?
The symptoms of prion diseases vary depending on the specific type and which parts of the brain are most affected, but they generally involve a rapid decline in neurological function. Initially, someone might experience subtle changes, but these quickly worsen. Common signs include a rapidly developing dementia, which means a swift decline in memory, thinking, and judgment, with individuals often forgetting day-to-day events and losing everyday skills.
People might also experience difficulty walking and changes in gait (ataxia), becoming unsteady on their feet, having trouble with balance, and their movements can become uncoordinated, leading to frequent falls. Jerking movements of the muscles (myoclonus) are common, appearing as sudden, involuntary muscle twitches that can be quite noticeable. Confusion and disorientation are also typical, with individuals struggling to recognize familiar people or objects, and often losing track of the day, date, or their surroundings. Personality changes, such as mood disturbances like aggression, irritability, anxiety, or depression, are frequent, and people might also show a lack of social judgment.
Difficulty speaking (dysarthria/aphasia) can manifest as slurred, quiet, or hard-to-understand speech, with word-finding difficulties increasing as the illness progresses, and some may even become completely mute. Hallucinations, where individuals see or hear things that are not there, can occur. Muscle stiffness (rigidity) and general fatigue are also common, and in specific types of prion disease, severe trouble sleeping (insomnia) can be a primary symptom. As the disease takes hold, individuals often lose the ability to care for themselves and may eventually enter a coma, as the progression is invariably fatal.
Mad Cow Disease: The Notorious Example
Perhaps the most famous, or infamous, prion disease is Bovine Spongiform Encephalopathy (BSE), widely known as “Mad Cow Disease.” This neurological disorder primarily affects cattle. Scientists believe the BSE epidemic that swept through the United Kingdom in the 1980s and 90s was caused by cattle eating feed that contained prion-infected products from other cows or sheep. When humans consumed meat from BSE-infected cows, they developed a human form of the disease known as variant Creutzfeldt-Jakob disease (vCJD).
The outbreak of Mad Cow Disease led to massive culling of cattle and strict regulations on animal feed worldwide to prevent contaminated tissues from entering the food chain. While cases are now extremely rare thanks to these measures, the memory of BSE serves as a stark reminder of the silent, potent threat that prions pose.
Beyond Mad Cow Disease, prions are also responsible for other conditions in animals like scrapie in sheep and chronic wasting disease (CWD) in deer, elk, and moose. In humans, other forms of prion diseases exist, some inherited, some sporadic (meaning they appear without a known cause), and some acquired through exposure.
Prevention and Control of Prions
Because prions are so resilient and can stay infectious in the environment for years, prevention and control are extremely challenging. Key measures focus on minimizing exposure to contaminated tissues. This includes strict feed bans to prevent feeding animal by-products to livestock, which was a major cause of the BSE outbreak. Rigorous screening and monitoring programs in livestock are in place to help detect and prevent the spread of prion diseases in animal populations.
There are also strict guidelines for the safe handling and disposal of tissues from suspected cases of prion disease in both medical and agricultural settings, especially high-risk tissues like the brain and spinal cord. Given that prions are resistant to normal sterilization methods like boiling, specialized chemical treatments such as strong hypochlorite solutions and high-temperature autoclaving are needed for instruments that have come into contact with infectious tissues, and disposable instruments are often preferred.
Furthermore, individuals with known or suspected prion disease cannot donate organs, tissues, or blood, as transmission can occur through these means (though human-to-human blood transmission has mainly been linked to vCJD). Lastly, people are advised to avoid consuming high-risk tissues from animals, such as brain and spinal cord, especially in areas where prion diseases might be present.
Treatment: A Tough Battle with No Cure Yet
This is the most challenging aspect of prion diseases: there is currently no known cure or effective treatment to stop or reverse their progression. All prion diseases are invariably fatal.
Current medical efforts focus primarily on alleviating symptoms and providing supportive care to improve the quality of life for affected individuals for as long as possible. This can involve medications to manage specific symptoms like muscle jerks, confusion, or insomnia. Patients often require extensive care, including assistance with daily activities, and may eventually need to move to specialized care facilities.
However, scientific research is ongoing, with scientists actively investigating various therapeutic approaches. Developing rapid and ultra-sensitive diagnostic tests (like RT-QuIC) is crucial for identifying the disease early, which could potentially open windows for future treatments. Researchers are exploring ways to stop the body from producing the normal prion protein (PrPC) using synthetic compounds like antisense oligonucleotides (ASOs), with studies in mice showing that preventing the production of this normal protein can significantly delay the onset of the disease.
Scientists are also looking for antibodies and small synthetic protein molecules that can directly block the conversion of normal prion protein into its abnormal, disease-causing form. Additionally, chemicals like hypochlorous acid are being investigated as potential disinfectants for prions in medical settings, as they are not toxic to humans but can destroy prions.
While there are no definitive breakthroughs yet, the dedication of researchers gives hope that one day, effective treatments or even preventative measures might be developed to combat these devastating protein-misfolding diseases.
Read Also: TY Danjuma Foundation Partners WHO with $2.26m Flexible Grant to Boost Health System in Nigeria